The year 2020 will forever be etched in the minds of those who lived to tell the tale. Oh, the stories we will tell. The smoke and mirrors were dispersed and the United States revealed its true self. We bore witness to Riot, after Riot, after Riot. The revolution appeared to be televised after all. But deep in our communities the true revolution was brewing. Many Black women and birthing people continued to give birth despite the headlines, the statistics, and the odds stacked against them. But they didn’t just give birth; they gave birth how they wanted, where they wanted, and focused on what was most important to them.
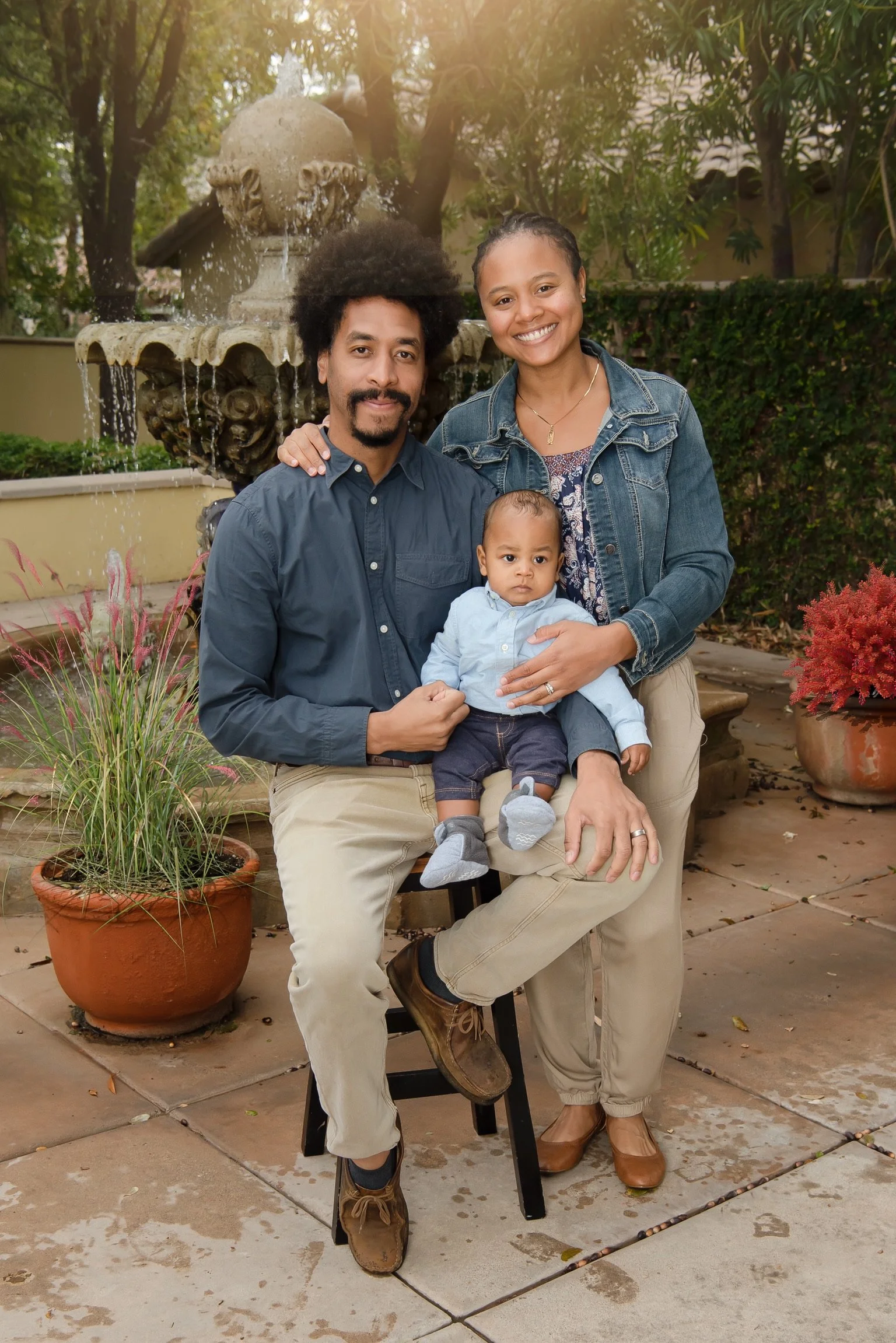
The Williams chose to keep their pregnancy to themselves aside from their parents. Their birth plans were kept under wraps and allowed them to keep out the noise, opinions, and outside stressors. Chris and Raquel chose a homebirth with a midwife and a doula.
Holistic care equipped Raquel with education, mental fortitude, and an understanding of what childbirth could include. When she started to feel the small ripples of early labor she contacted her birth team which included her midwife, doula, and birth photographer. Chris was spending the day attending graduation ceremonies for his students. Raquel told Chris he was fine to go and she knew it would be fine. They had a late dinner but didn’t set up the birthing tub because it was too late in the day. The waves were not close enough for her to think that she was in active labor. She checked in with her midwife and she told her to use her discernment. Raquel took a Tylenol PM and they enjoyed a movie and facials until she fell asleep. Around four in the morning, Raquel stated that she had to poop. They went down together, Chris could see her from the door, and as Raquel made a maneuver he said, “I don’t think that’s poop.” Chris was scared that the baby had died, due to the shape and stillness of her head. Meanwhile, Raquel was in a calm, zen state as she assured Chris the baby was ok. They were able to Facetime their midwife to manage the delivery of the baby. Chris caught their baby with a nuchal cord and unwrapped it and placed the baby on Raquel’s chest. The midwife entered the house shortly after. Dani and the birth photographer joined them shortly afterward for postpartum support and photography.
Immediately postpartum, they walked back down the hall with their baby. The experience of having their team come to them and the care that was provided for them had them in awe. Raquel believes that everything we need to have children… we already have it. We’ve been having babies like this forever.
Read More